Free Printable Nursing Handoff Report Template Printable Form
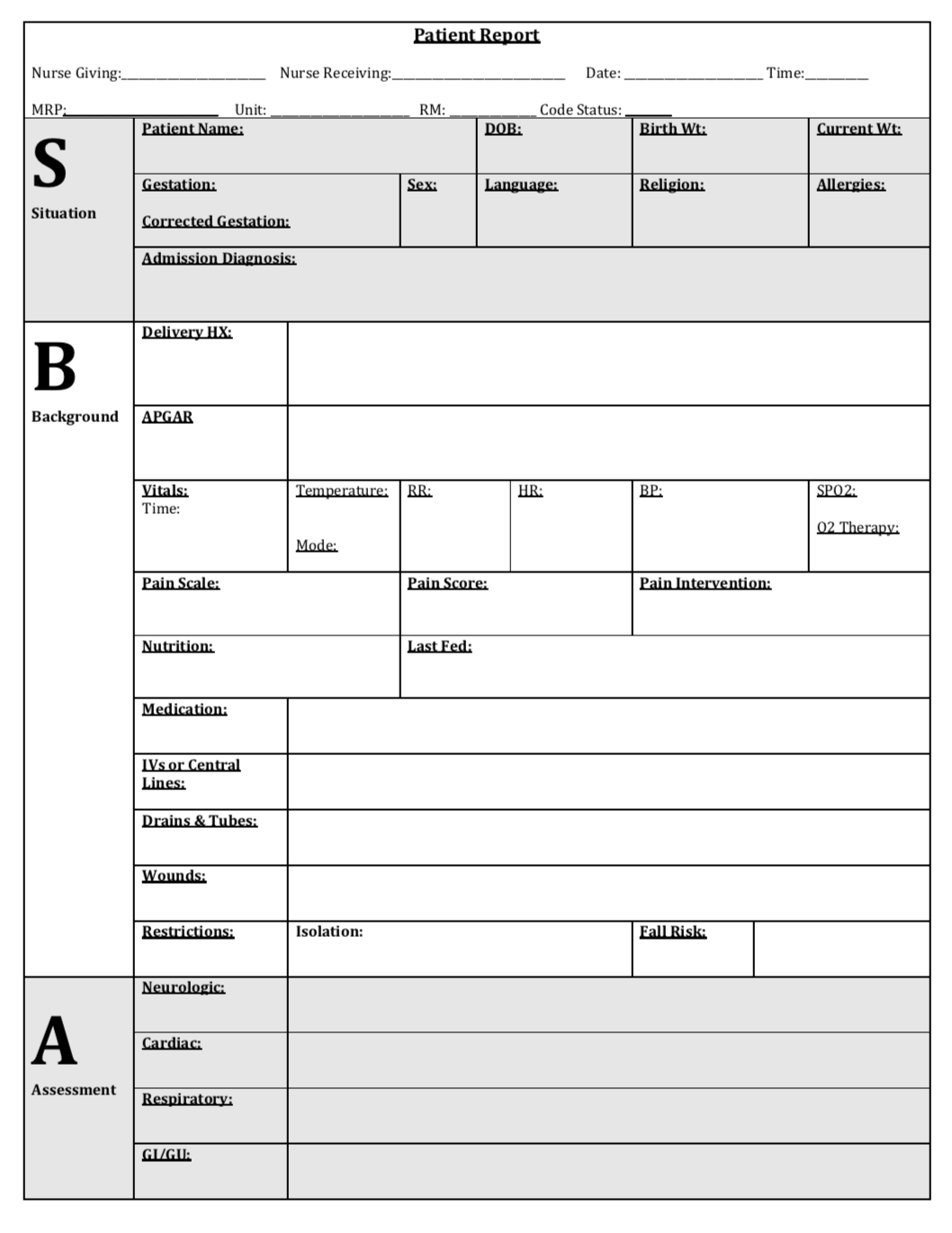
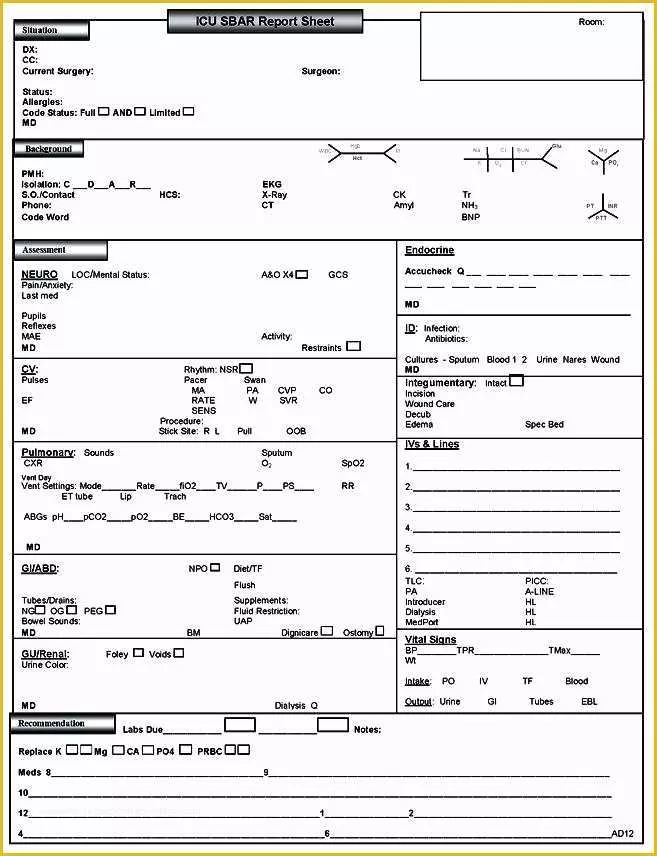
SBAR Patient Report Newborn Simulation
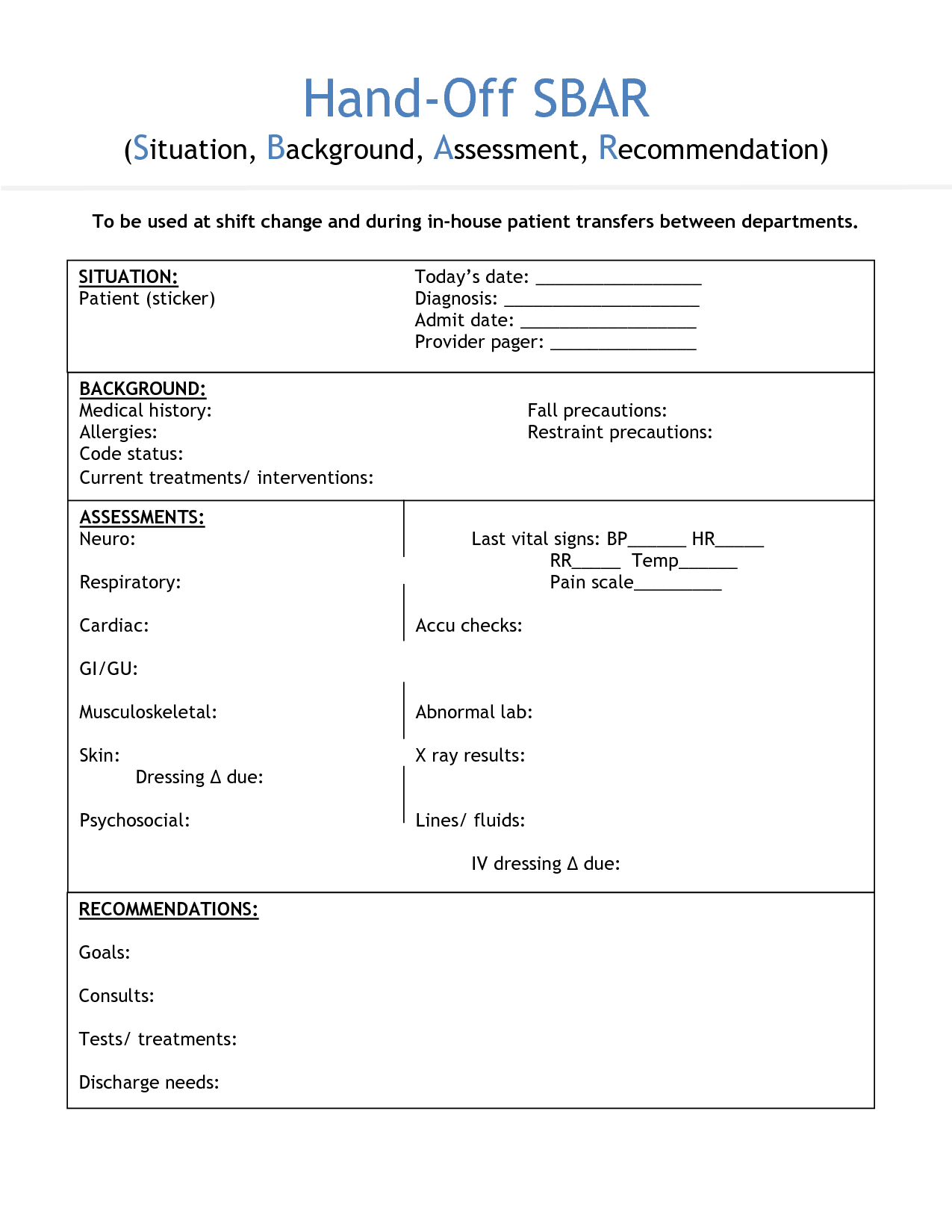
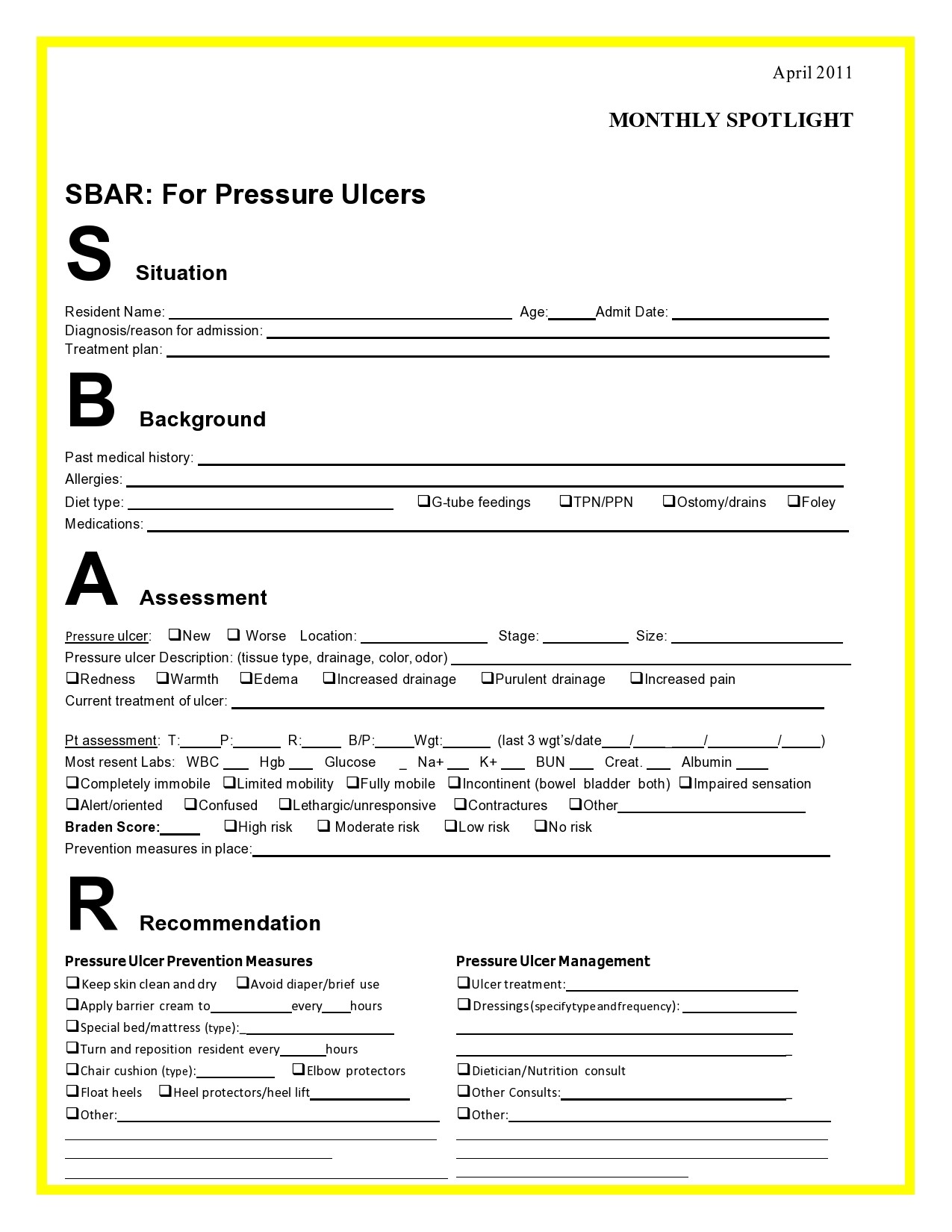
Download this free SBAR template to efficiently document the Situation, Background, Assessment, and Recommendation about a particular patient or case. Using this template, be able to completely provide information to help ensure continuity of patient care by doing the following:

Sbar Template Word Business Design Layout Templates
An SBAR report is a tool of communication between members of the healthcare team about a client's condition that follows the SBAR communication technique. SBAR stands for: S ituation B ackground A ssessment R ecommendation What is the purpose of the SBAR technique?
free sbar template for nurses Sbar Report Sheet Template Nurse report
SBAR stands for Situation, Background, Assessment, and Recommendation—an effective framework for conveying critical information between healthcare professionals. Our customizable and printable templates provide a structured approach to communicate patient conditions, vital signs, medical history, and recommended actions.
Sbar Report Template
Safer Care SBAR Situation • Background • Assessment • Recommendation Implementation and Training Guide

Paper & Party Supplies Stationery Nurse Report Sheet SBar & Brain
An SBAR Report Template serves as a structured framework for facilitating clear and effective communication among healthcare professionals regarding a patient's condition, particularly in situations demanding prompt intervention.
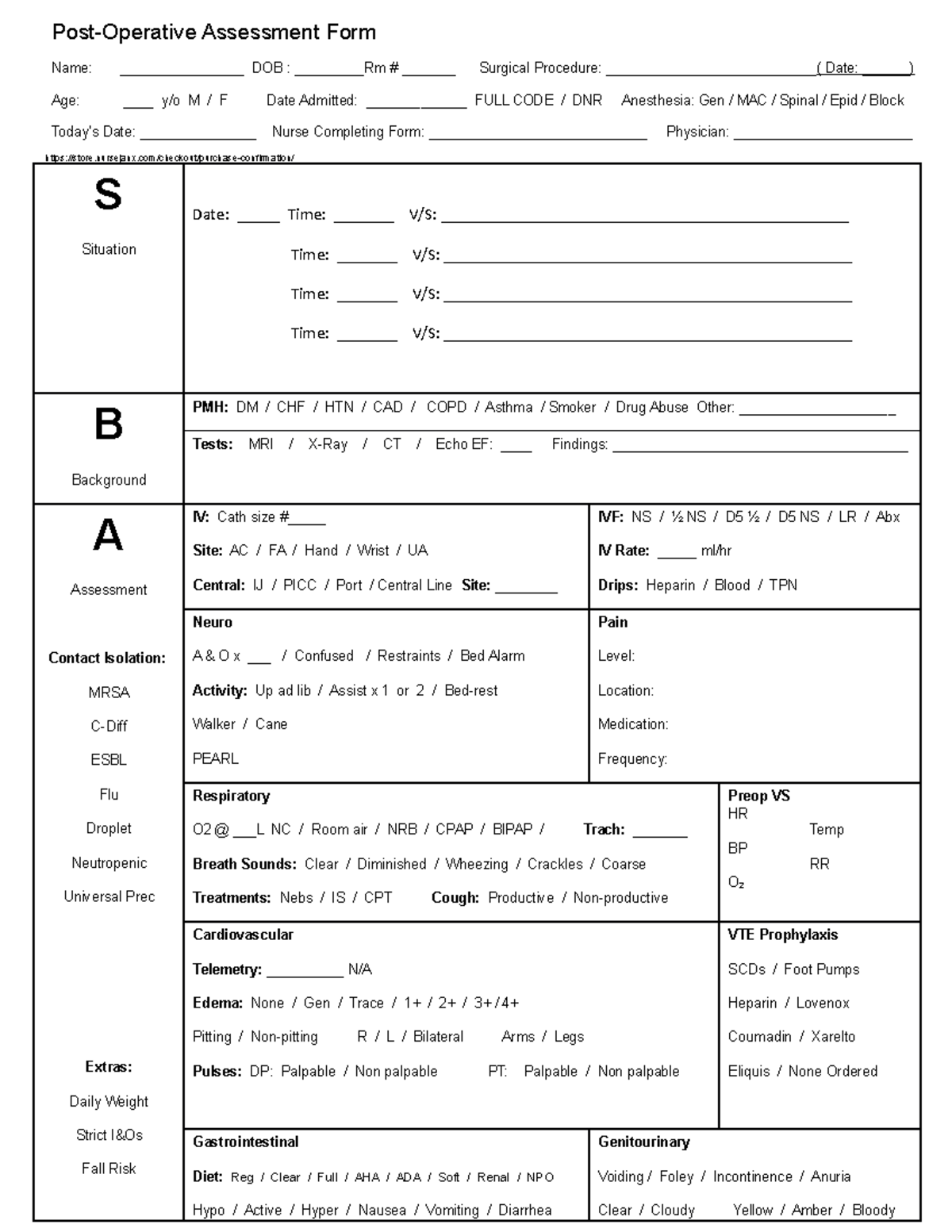
Sbar Fullsize Nursing Report Sheet Op Assessment Studocu Vrogue
13 Blank SBAR Templates (Word, PDF) SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals.
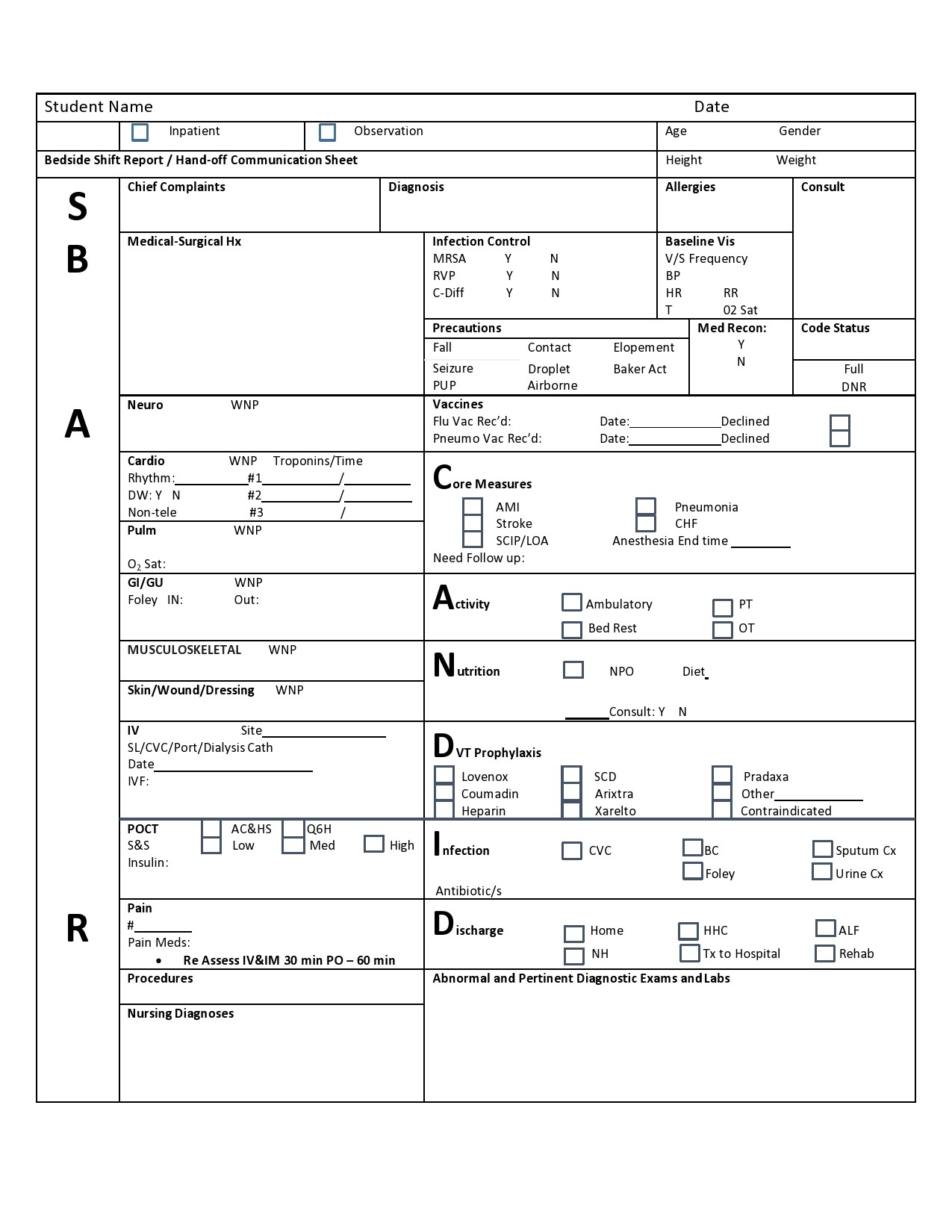
Free Printable Nursing Handoff Report Template Printable Form
SBAR is an easy to remember mechanism that you can use to frame conversations, especially critical ones, requiring a clinician's immediate attention and action. It enables you to clarify what information should be communicated between members of the team, and how. It can also help you to develop teamwork and foster a culture of patient safety.
Free Printable Sbar Template Of Nursing Handoff Report Sheet Beautiful
Free downloadable tools to support your work to improve health care quality and safety at every stage — from establishing a project plan and an improvement aim, to understanding a process, to identifying root causes or drivers, to testing changes using PDSA cycles, to implementing and spreading successful improvements, and more. Featured Tools

Free download! This is a fullsize SBAR nursing brain report sheet. 1
The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition. SBAR is an easy-to-remember, concrete mechanism useful for framing any conversation, especially critical ones, requiring a clinician's immediate attention and action.

Sbar Nursing Shift Report Form On Sbar Nursing Worksheet Med Surg
SBAR Worksheet ("SBAR report to physician about a critical situation"): A worksheet/script that a provider can use to organize information in preparation for communicating with a physician about a critically ill patient
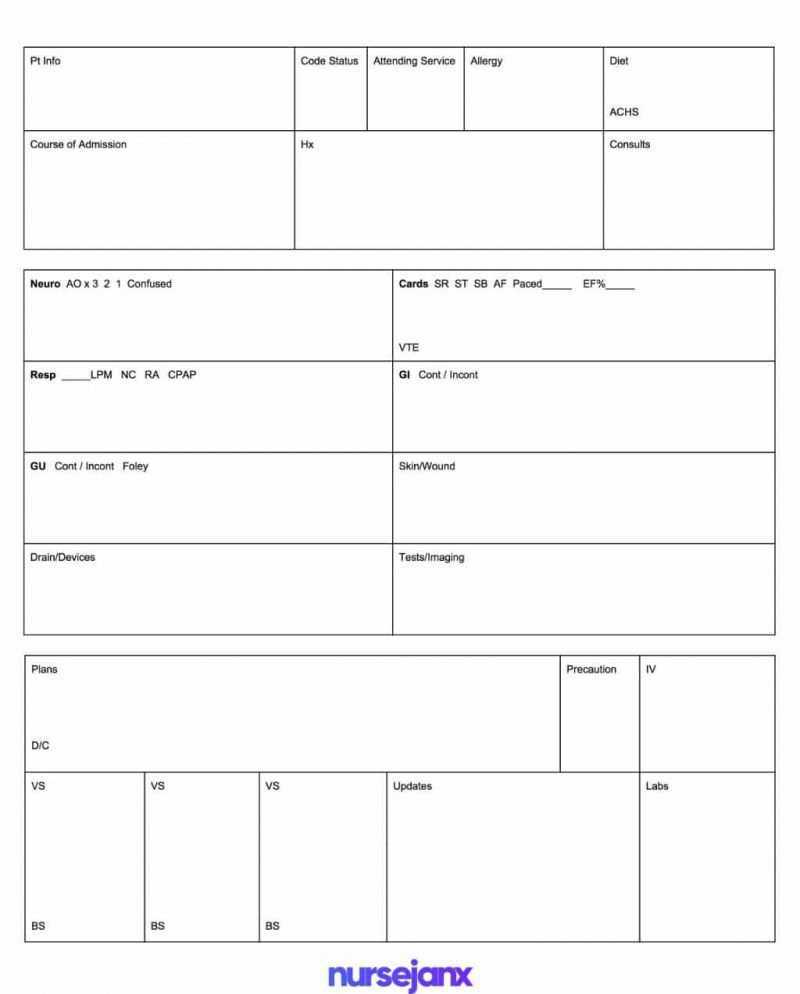
Best Free Sbar & Brain Nursing Report Sheet Templates Inside Nurse
The SBAR (Situation, Background, Assessment, Recommendation) tool is used by all nursing fields within primary and secondary healthcare environments to aid patient safety ( NHS Improvement, 2018 ). Acts of communication through handovers, ward rounds, shift exchanges and team meetings are examples of when information is exchanged between nurses.
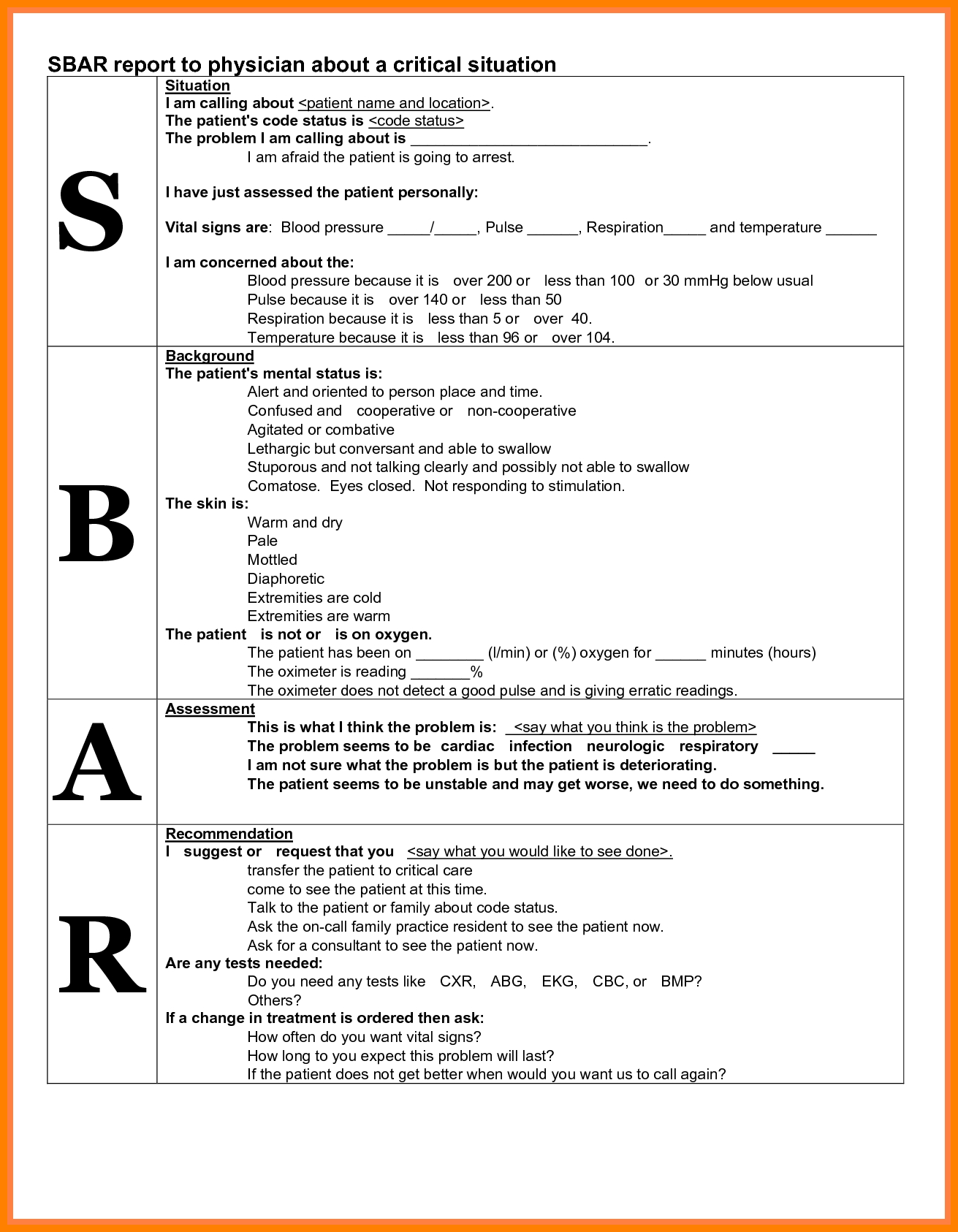
Sbar Examples Nurse To Doctor One Checklist That You Should Keep In
What is SBAR? SBAR is a standard to communicate medical information. Simply, it improves accuracy and helps to correct dangerous errors. It Stands for: (Situation, Background, Assessment, Recommendation) The above four terms are the key facts. However, all should be conveyed properly.
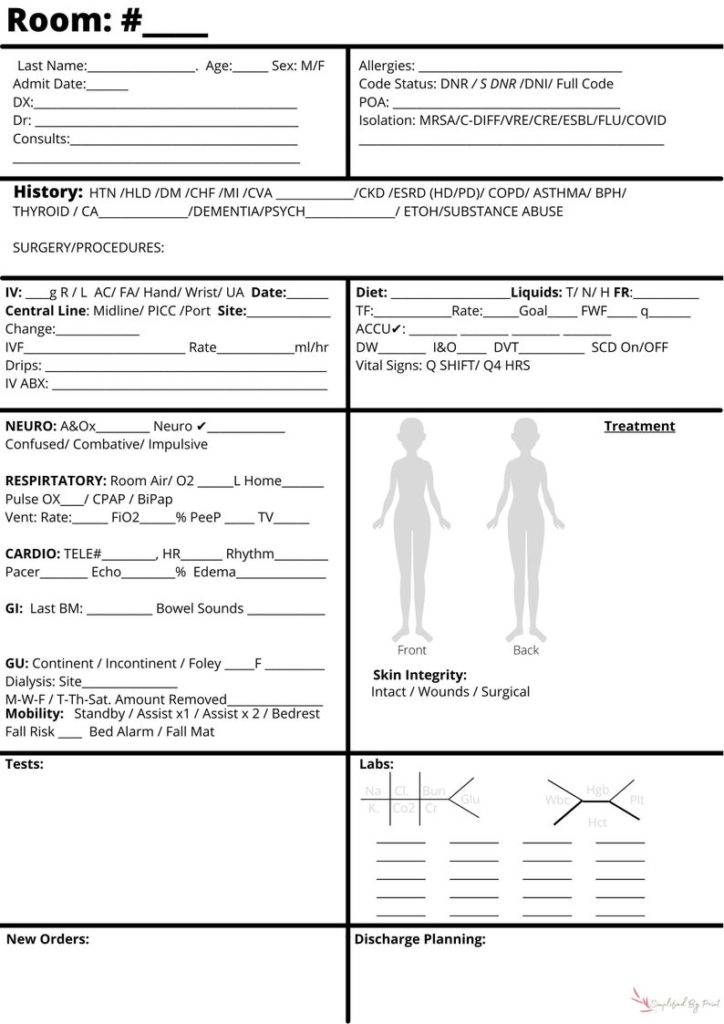
Nursing SBAR Bedside Report Sheet Simplified by Print
How to Create your SBAR Nurse Report Sheet. You can generate a PDF printout (just like the screenshot above) using the NurseBrain app (available on IOS and Android ). Just open the NurseBrain app, go to your clipboard, swipe right on the patient you want to share and select "Share PDF.". If the incoming nurse already has the NurseBrain app.

Printable Blank Sbar Template
SBAR (Situation, Background, Assessment, Recommendation) is a verbal or written communication tool that helps provide essential, concise information, usually during crucial situations. In some cases, SBAR can even replace an executive summary in a formal report because it provides focused and concise information.
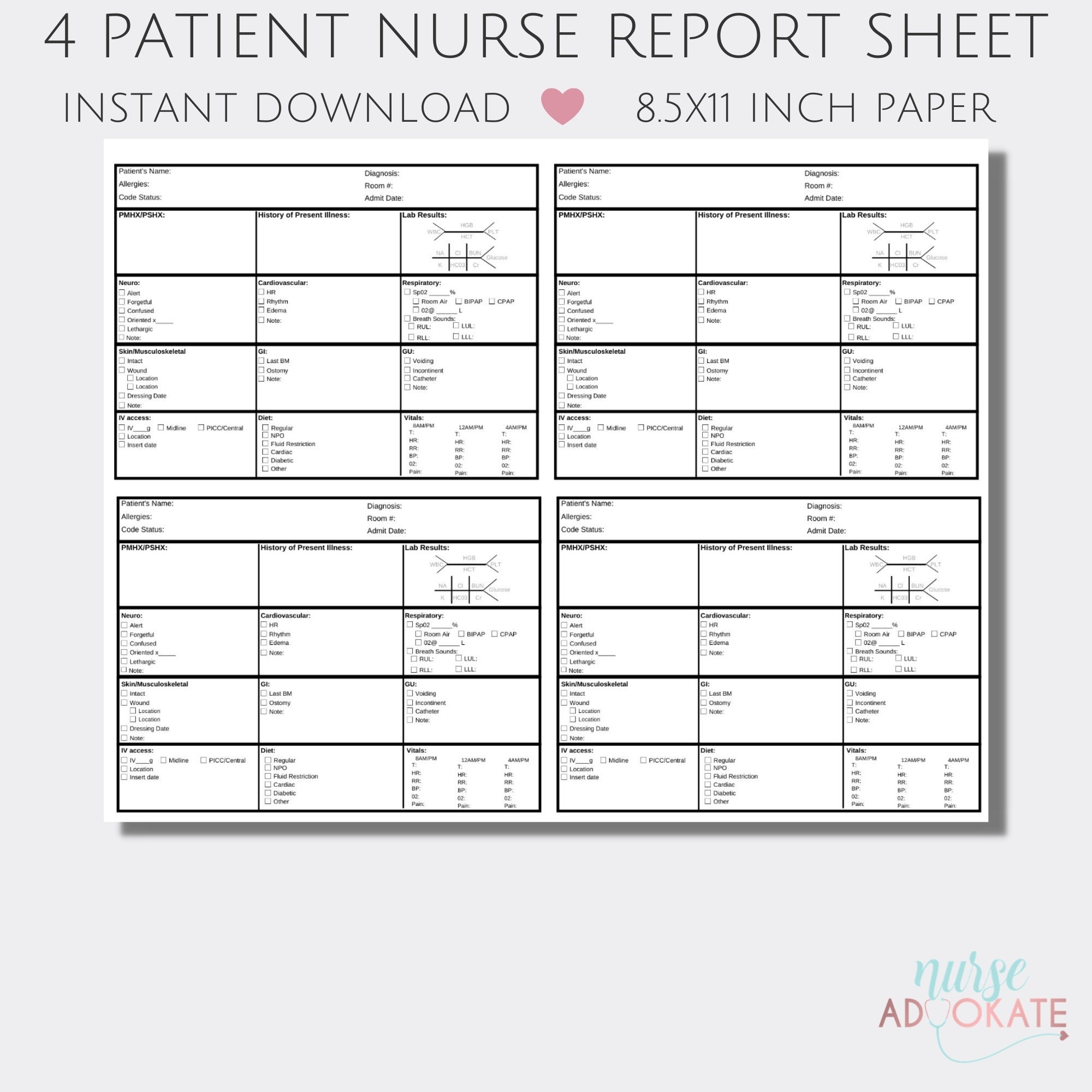
nursing report sheet b etsy 4 patient night shift report sheet nurses
NHS England and NHS Improvement SBAR communication tool - situation, background, assessment, recommendation What is it? SBAR is an easy to use, structured form of communication that enables information to be transferred accurately between individuals.

Nurses Report Sheet Nurse Report Sheet Nurse Brain Sheet Sbar Images
SBAR ( s ituation, b ackground, a ssessment, r ecommendation) was designed as a communication tool to convey critical information requiring immediate action and advice. It has been adopted widely in healthcare settings as a structured method of communicating important clinical information (e.g. escalation of care, patient handover).